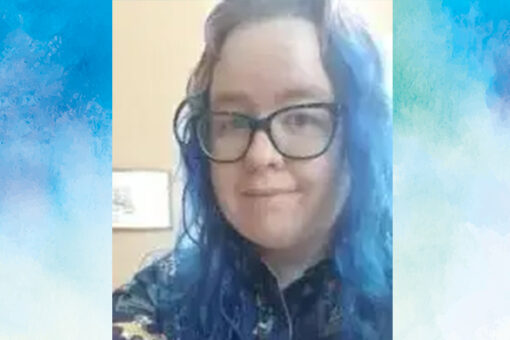
At Center for Discovery, we are grateful to have had the opportunity to hear from our alum of CFD Atlanta, Tori Anderson. Tori opens up about their experience with autism, eating disorders, working their recovery, and what has helped them get to where they are today. Here’s Tori’s inspiring story:
Q: What was life like before your autism diagnosis?
A: I was diagnosed at the age of 25, although I had inklings of being autistic from the age of 13 or so. In the times before I was officially diagnosed, I was told that I couldn’t be autistic for I did not have a lot of the stereotypical traits as many traits present differently in AFABs (assigned female at birth) than in AMABs (assigned male at birth); so, I was forced to learn to mask what traits I had and appear more “neurotypical.”
I was brutally bullied throughout school and struggled socially and with the pressure of masking, I struggled mentally to the point that I developed eating disorders and other mental health conditions. Much of my growing up and early adulthood was trying to figure out how to “fit in” in a society that wasn’t made for people like me, especially as I was constantly told I couldn’t be autistic because I didn’t “appear” autistic. It is wild to grow up being told you can’t be neurodivergent, but actually are neurodivergent and learning how to navigate life being completely inauthentic until finally being told what you thought of yourself was actually true.
Q: When did you realize you had an eating disorder? What kind of eating disorder are you healing from?
A: So, I actually have two competing eating disorders. I have always had a difficulty with food but thinking back, I realized I started exhibiting traits of atypical anorexia nervosa (AAN) when I was about 14. I started restricting considerably around then because of the pressures of masking and being bullied for my size. I was officially diagnosed with AAN when I was 24 after an inpatient psych stay. This is the eating disorder I was treated for while at CFD.
Recently (in the last few months) at the age of 27, I relapsed and suddenly was unable to eat a large variety of foods. This made it clear to me and my outpatient team that I also struggle with avoidant restrictive food intake disorder (ARFID), specifically the sensory repulsive type. This is something that my outpatient dietitian noticed when we started working together after my first time at CFD (she was made aware of my sensory issues by the CFD dietitian who recommended her to me and in our work together). My dietitian has always taken into account my ARFID symptoms in our work, but it wasn’t until I was aware of it being an issue, as well, did we start to really work on it along with the AAN.
Q: How, if at all, has your eating disorder and autism intersected?
A: Both of my eating disorders are results of being autistic. AAN is from the pressure of masking and caring way too much to fit in. When I did eat, I would force myself to just eat what others were eating as a teenager/early adulthood. ARFID came from a relapse that happened after starting an unmasking (or learning how to be authentically autistic) journey and I realized that a majority of foods have some level of riskiness/not feeling safe due to sensory avoidances through texture, taste and visuals.
Q: For those who don’t know, can you explain what autistic burnout is?
A: According to an article written by Dr. Megan Neff, autistic burnout is often a result of living inauthentically or more like neurotypicals. There are three main traits of autistic burnout: chronic exhaustion, decrease in the ability to tolerate sensory stimuli, and a regression of mental abilities (Neff, 2023). It can act similarly to depression from an outsider’s perspective but needs to be treated differently than traditional depression.
Q: How did learning about autistic burnout help you cope? What are your go-to coping skills for autistic burnout and treatment?
A: Learning about autistic burnout from “actually autistic” creators, mainly on social media like Instagram, has led to a newer approach in handling my mental health. Before, I struggled very severely while trying traditional depression coping skills and methods like taking antidepressants. These traditional methods made me feel like I was just trapped and couldn’t be fixed because nothing worked even after taking med after med and doing all the treatment. Dialectical behavioral therapy (DBT) helped some, to have set skills to use in different moments and understanding that opposites could co-occur. It was much more helpful than traditional talk therapy and I am grateful to CFD for introducing it to me.
After learning about autistic burnout, I discovered that I needed to take a different approach to handle my mental health. The main coping skills I learned to handle autistic burnout is to be more authentically autistic. To do so, I have learned to be more attentive to my sensory needs and take sensory breaks (my favorite method is to listen to music with headphones and cuddle stuffed animals) when needed and actually stim more. Stimming is a name for self-regulating motions that help to calm all people down (not just neurodivergent folks). My favorite stims are listening to music and tapping my foot or when feeling okay enough, dancing along with it; playing with fidget toys (whether designed fidget toys or other objects like pencils/pens); and stroking/cuddling with stuffed animals. One thing that I have done in my unmasking journey is allow myself to bring a stuffed animal with me in most places. Bringing one in treatment was so comforting and was a major way I was able to get through treatment.
Q: What has life been like for you after treatment at CFD?
A: Life has been interesting since leaving CFD. I’m grateful for alumni groups to help me get support while out of treatment, as the eating disorders are still a challenge. Though, it is getting easier as I continue on my unmasking journey, which was included in my second time at CFD as my autism was more accepted. It is always helpful to have communities to be a part of. I left CFD and got a new job as a Direct Support Professional (which is essentially a carer) for a day center for disabled adults who have helped me accept my own disabilities and work to help them get their voices heard.
Q: What kind of advice would you give to someone who has autism and is also working through eating disorder recovery? What would you say to their loved ones?
A: Let your autism be known. It will be best to be accommodated. Autism plays into ED recovery so much and you need to be open to have those connection conversations. I thought at first that my autism and eating disorders were separate entities but definitely not. The further I move into my ED recovery journey, the more I realize how interconnected autism and eating disorders are for me; nothing wrong with that. Be vocal about needing breaks if you get overstimulated and have aids with you (and actually use them). There were times in treatment that I would just shutdown because of forcing too much to work through too much sensory input. I would say something and a staff member would take me to a quiet room and encourage me to use aids and it helped so much. EDs are hard and being autistic can be hard, but being prepared and taking breaks before shutdowns/meltdowns will help so much and make the process easier.
For loved ones, it is imperative that you listen to your autistic loved one. They aren’t lying when foods can have sensory icks for them and that can be a reason for food to be challenging even if they don’t have ARFID. Encourage them to advocate for themselves or advocate for them to get accommodations for their autism while in treatment and in everyday life. Let them have sensory breaks (ED recovery/treatment can be very overstimulating). Listen to the voices of actually autistic people (search for #actuallyautistic on social media like Instagram and TikTok) and autistic-led organizations like Autistic Women and Nonbinary Network (AWN) or Autistic Self Advocacy Network (ASAN). Educate yourself the best you can from these resources.
Q: What do you see for yourself in the near future? What are you looking forward to?
A: Although I’m not sure what I want to do at the moment, I look forward to being an advocate for people like me. ED recovery is much more of an achievable place for me now that I have accepted and worked with being autistic than trying to fight it. I also look forward to getting married soon and am grateful for loved ones like my partner for accepting me and encouraging me to try different methods/avenues of getting help.
Tori Anderson (they/them) is an actually autistic adult living in Georgia. They have been through CFD treatment a couple of times (once residential and PHP and the other PHP/IOP). They try to advocate for themselves and others like them to help others get through difficult challenges.
Resources
Neff, M. A. (2023, July 11). Autism and Burnout. Insights of a Neurodivergent Clinician. https://neurodivergentinsights.com/autism-infographics/autism-and-burnout